Treatment: If the patient is unconscious call 911 immediately then perform CPR—if the patient is a child or infant perform CPR for 2 minutes and then call 911. Make sure to lay the patient down with his/her feet 12 inches above the heart. Check for C-A-B’s. You may need to put the patient on his/her side to prevent choking. Make sure to check for other injuries.
When a Seizure occurs, these are signs to look for: dizziness or faintness, uncontrolled bowel movement, breathing difficulties, unconsciousness or unresponsiveness, arching of the back, clenching of things—such as teeth. If a patient is ever unconscious or unresponsive, make sure to perform CPR and to call 911. Some causes of Seizures are head injuries, fevers, brain damage, poisoning, cessation of oxygen to the brain and diabetes.
Treatment: check universal precautions, remove any life-threatening objects, loosen clothing, and make sure to call 911 and respond with appropriate orders. Make sure NOT to restrain the patient unless the patient is going to be hurt or is going to hurt someone.
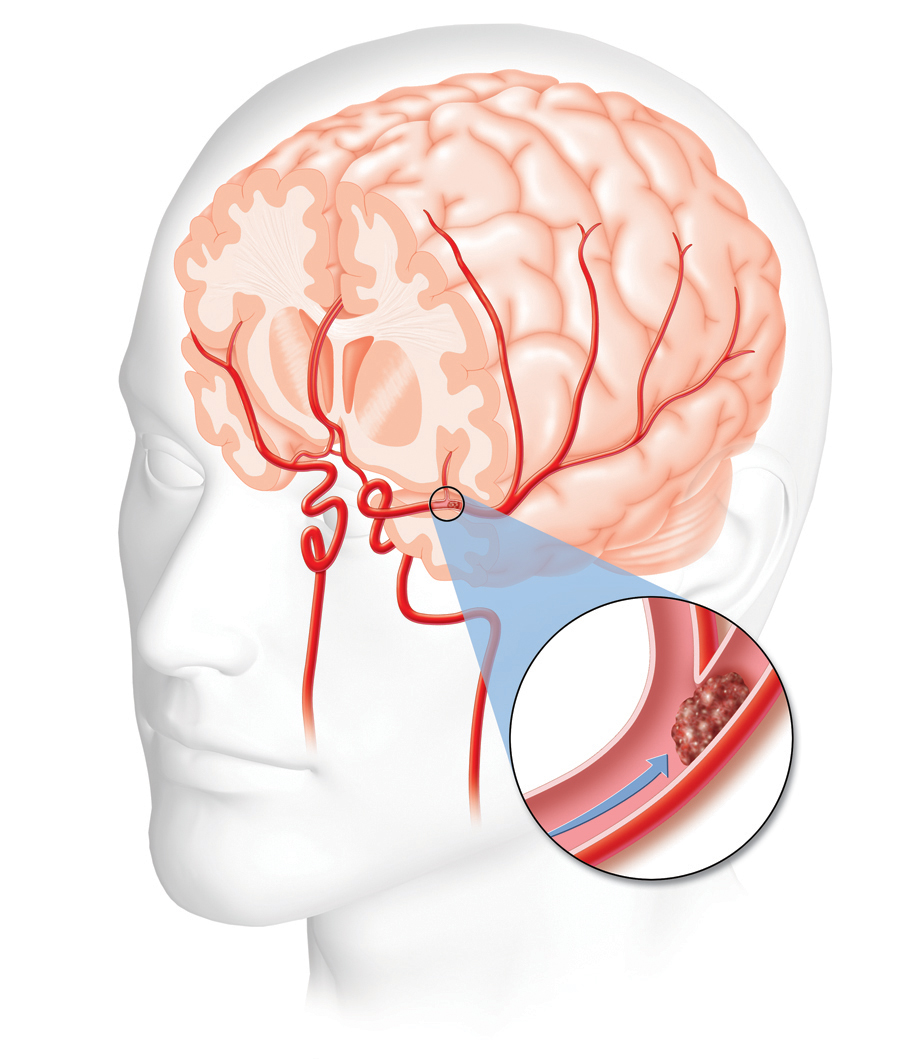
A Stroke occurs when there is a ruptured/blocked blood vessel in the brain. The brain begins deteriorating when it has a cessation of oxygen. If the patient falls unconscious or is unresponsive, call 911 and perform CPR immediately. It is recommended for first-aid providers to use a stroke assessment system. A System such as Cincinnati Prehospital Stroke Scale (CPSS) is a simple tool when assessing a stroke patient. CPSS Stroke Scale:
Facial droop assessment:
To check: ask patient to smile
Normal: patient’s cheeks move equally on both sides
Abnormal: patient's face moves unequally on both sides
Arm drift assessment:
To check: have patient raise arms at shoulder length for 10 seconds
Normal: both arms equally move together (another condition might occur: pronator drift)
Abnormal: arms fail to respond equally
Speech assessment:
To check: ask patient a question
Normal: patient does not slur and answers correctly
Abnormal: patient is mute, using abnormal words and/or slurring
If 1 out of the three examinations occurs there is a 72% probability of a stroke.
Risk factors: high blood pressure, heart disease, diabetes, smoking and having had a prior stroke.